Services
Services We Provide
Chicago Foot Health Centers
can assist with many different foot issues
that may occur. Our doctors can treat anything from bunions and heel pain to ankle injuries and diabetic foot care. Give us a call today to schedule your appointment for treatment!

Bunions
A
bunion is an enlargement of the joint at the base of the big toe—the metatarsophalangeal (MTP) joint—that forms when the bone or tissue at the big toe joint moves out of place. This forces the toe to bend toward the others, causing an often painful lump of bone on the foot. Since this joint carries a lot of the body's weight while walking, bunions can cause extreme pain if left untreated. The MTP joint itself may become stiff and sore, making even the wearing of shoes difficult or impossible.
Read More
Symptoms
• Development of a firm bump on the outside edge of the foot, at the base of the big toe.
• Redness, swelling, or pain at or near the MTP joint.
• Corns or other irritations caused by the overlap of the first and second toes.
• Restricted or painful motion of the big toe.
How Do You Get a Bunion? Bunions form when the normal balance of forces that is exerted on the joints and tendons of the foot becomes disrupted. This can lead to instability in the joint and cause the deformity. They are brought about by years of abnormal motion and pressure over the MTP joint. They are, therefore, a symptom of faulty foot development and are usually caused by the way we walk, and our inherited foot type, our shoes, or other sources. People who suffer from flat feet or low arches are also prone to developing these problems, as are arthritic patients and those with inflammatory joint disease. Occupations that place undue stress on the feet are also a factor; ballet dancers, for instance, often develop the condition. Wearing shoes that are too tight or cause the toes to be squeezed together is also a common factor, one that explains the high prevalence of the disorder among women.
What Can You Do For Relief? Apply a commercial, non-medicated bunion pad around the bony prominence. Wear shoes with a wide and deep toe box. If your bunion becomes inflamed and painful, apply ice packs several times a day to reduce swelling. Avoid high-heeled shoes over two inches tall. See your podiatric physician if pain persists. Pain Treatment options vary with the type and severity of each bunion, although identifying the deformity early in its development is important in avoiding surgery. Podiatric medical attention should be sought at the first indication of pain or discomfort because, left untreated, bunions tend to get larger and more painful, making nonsurgical treatment less of an option. The primary goal of most early treatment options is to relieve pressure on the bunion and halt the progression of the joint deformity. At Chicago Foot Health Centers, we may recommend these treatments:
• Padding & Taping -- Often the first step in a treatment plan, padding the bunion minimizes pain and allows the patient to continue a normal, active life. Taping helps keep the foot in a normal position, thus reducing stress and pain.
• Medications -- Anti-inflammatory drugs and cortisone injections are often prescribed to ease the acute pain and inflammations caused by joint deformities.
• Physical Therapy -- Often used to provide relief of the inflammation and from bunion pain. Ultrasound therapy is a popular technique for treating bunions and their associated soft tissue involvement.
• Orthotics -- Shoe inserts may be useful in controlling foot function and may reduce symptoms and prevent worsening of the deformity. When early treatments fail or the bunion progresses past the threshold for such options, podiatric surgery may become necessary to relieve pressure and repair the toe joint.
Surgical Options When conservative treatment does not provide satisfactory relief from symptoms, or when the condition interferes with your activities, surgery may be necessary. Pain and deformity are significantly reduced in the great majority of patients who undergo bunion surgery. The surgery will remove the bony enlargement, restore the normal alignment of the toe joint, and relieve pain. Postoperative orthoses or supportive devices may be recommended to improve foot function. Surgery may be performed at a hospital, surgical center or properly equipped office operating room. Depending on the procedure, the facility at which it is performed and the patient's medical status, the surgeon may choose a local, spinal or general anesthetic. In many cases, the procedure can be performed under local anesthesia.
• Development of a firm bump on the outside edge of the foot, at the base of the big toe.
• Redness, swelling, or pain at or near the MTP joint.
• Corns or other irritations caused by the overlap of the first and second toes.
• Restricted or painful motion of the big toe.
How Do You Get a Bunion? Bunions form when the normal balance of forces that is exerted on the joints and tendons of the foot becomes disrupted. This can lead to instability in the joint and cause the deformity. They are brought about by years of abnormal motion and pressure over the MTP joint. They are, therefore, a symptom of faulty foot development and are usually caused by the way we walk, and our inherited foot type, our shoes, or other sources. People who suffer from flat feet or low arches are also prone to developing these problems, as are arthritic patients and those with inflammatory joint disease. Occupations that place undue stress on the feet are also a factor; ballet dancers, for instance, often develop the condition. Wearing shoes that are too tight or cause the toes to be squeezed together is also a common factor, one that explains the high prevalence of the disorder among women.
What Can You Do For Relief? Apply a commercial, non-medicated bunion pad around the bony prominence. Wear shoes with a wide and deep toe box. If your bunion becomes inflamed and painful, apply ice packs several times a day to reduce swelling. Avoid high-heeled shoes over two inches tall. See your podiatric physician if pain persists. Pain Treatment options vary with the type and severity of each bunion, although identifying the deformity early in its development is important in avoiding surgery. Podiatric medical attention should be sought at the first indication of pain or discomfort because, left untreated, bunions tend to get larger and more painful, making nonsurgical treatment less of an option. The primary goal of most early treatment options is to relieve pressure on the bunion and halt the progression of the joint deformity. At Chicago Foot Health Centers, we may recommend these treatments:
• Padding & Taping -- Often the first step in a treatment plan, padding the bunion minimizes pain and allows the patient to continue a normal, active life. Taping helps keep the foot in a normal position, thus reducing stress and pain.
• Medications -- Anti-inflammatory drugs and cortisone injections are often prescribed to ease the acute pain and inflammations caused by joint deformities.
• Physical Therapy -- Often used to provide relief of the inflammation and from bunion pain. Ultrasound therapy is a popular technique for treating bunions and their associated soft tissue involvement.
• Orthotics -- Shoe inserts may be useful in controlling foot function and may reduce symptoms and prevent worsening of the deformity. When early treatments fail or the bunion progresses past the threshold for such options, podiatric surgery may become necessary to relieve pressure and repair the toe joint.
Surgical Options When conservative treatment does not provide satisfactory relief from symptoms, or when the condition interferes with your activities, surgery may be necessary. Pain and deformity are significantly reduced in the great majority of patients who undergo bunion surgery. The surgery will remove the bony enlargement, restore the normal alignment of the toe joint, and relieve pain. Postoperative orthoses or supportive devices may be recommended to improve foot function. Surgery may be performed at a hospital, surgical center or properly equipped office operating room. Depending on the procedure, the facility at which it is performed and the patient's medical status, the surgeon may choose a local, spinal or general anesthetic. In many cases, the procedure can be performed under local anesthesia.

Hammer Toes & Corns
A hammer toe deformity is a contracture of the toe(s). In this condition, the toe is bent at the middle joint, so that it is buckled or hammered. Initially, hammer toes are flexible and can be corrected with simple measures but, if left untreated, they can become fixed and require surgery. People with hammer toes may have corns or calluses on the top of the middle joint of the toe or on the tip of the toe. They may also feel pain in their toes or feet and have difficulty finding comfortable shoes.
Read More
Causes of hammer toes Hammer toes result from shoes that don't fit properly or a muscle imbalance, usually in combination with one or more other factors. Muscles work in pairs to straighten and bend the toes. If the toe is bent and held in one position long enough, the muscles tighten and cannot stretch out. Shoes that narrow toward the toe may make your forefoot look smaller. But they also push the smaller toes into a flexed (bent) position. The toes rub against the shoe, leading to the formation of corns and calluses, which further aggravate the condition. A higher heel forces the foot down and squishes the toes against the shoe, increasing the pressure and the bend in the toe. Eventually, the toe muscles become unable to straighten the toe, even when there is no confining shoe.
Treatment for hammertoes Conservative treatment starts with new shoes that have soft, roomy toe boxes. Shoes should be one-half inch longer than your longest toe. (Note: For many people, the second toe is longer than the big toe.) Avoid wearing tight, narrow, high-heeled shoes. You may also be able to find a shoe with a deep toe box that accommodates the hammer toe. Or, a shoe repair shop may be able to stretch the toe box so that it bulges out around the toe. Sandals may help, as long as they do not pinch or rub other areas of the foot. Your doctor may recommend that you use commercially available straps, cushions or non-medicated corn pads to relieve symptoms. You should try to avoid all medicated corn pads as they usually do more harm than good. If you have diabetes, poor circulation or a lack of feeling in your feet, avoid any forms of self-treatment and visit a podiatrist. Hammertoes can be corrected by surgery if conservative measures fail. Usually, surgery is done on an outpatient basis with a local anesthetic. The actual procedure will depend on the type and extent of the deformity. After the surgery, there may be some stiffness, swelling and redness and the toe may be slightly longer or shorter than before. You will be able to walk but should not plan any long hikes while the toe heals, and should keep your foot elevated as much as possible.
Treatment for hammertoes Conservative treatment starts with new shoes that have soft, roomy toe boxes. Shoes should be one-half inch longer than your longest toe. (Note: For many people, the second toe is longer than the big toe.) Avoid wearing tight, narrow, high-heeled shoes. You may also be able to find a shoe with a deep toe box that accommodates the hammer toe. Or, a shoe repair shop may be able to stretch the toe box so that it bulges out around the toe. Sandals may help, as long as they do not pinch or rub other areas of the foot. Your doctor may recommend that you use commercially available straps, cushions or non-medicated corn pads to relieve symptoms. You should try to avoid all medicated corn pads as they usually do more harm than good. If you have diabetes, poor circulation or a lack of feeling in your feet, avoid any forms of self-treatment and visit a podiatrist. Hammertoes can be corrected by surgery if conservative measures fail. Usually, surgery is done on an outpatient basis with a local anesthetic. The actual procedure will depend on the type and extent of the deformity. After the surgery, there may be some stiffness, swelling and redness and the toe may be slightly longer or shorter than before. You will be able to walk but should not plan any long hikes while the toe heals, and should keep your foot elevated as much as possible.

Heel Pain
Heel Pain is one of the most common disorders we treat at Chicago Foot Health Centers. Usually it occurs beneath the heel or behind the heel. If it hurts under your heel, you may have one or more conditions that inflame the tissues on the bottom of your foot:
• Plantar fasciitis (sub calcaneal pain):
Doing too much running or jumping can inflame the tissue band (fascia) connecting the heel bone to the base of the toes. The pain is centered under your heel and may be mild at first but flares up when you take your first steps after resting overnight.
• Heel spur:
When plantar fasciitis continues for a long time, a heel spur (calcium deposit) may form where the fascia tissue band connects to your heel bone. Your doctor may take an X-ray to see the bony protrusion, which can be 1/4" or longer.
Read More
Plantar Fasciitis
When your first few steps out of bed in the morning cause severe pain in the heel of your foot, you may have plantar fasciitis (fashee-EYE-tiss). It's an overuse injury affecting the sole or flexor surface (plantar) of the foot. A diagnosis of plantar fasciitis means you have inflamed the tough, fibrous band of tissue (fascia) connecting your heel bone to the base of your toes. You're more likely to get the condition if you're a woman, if you're overweight, or if you have a job that requires a lot of walking or standing on hard surfaces. You're also at risk if you walk or run for exercise, especially if you have tight calf muscles that limit how far you can flex your ankles. People with very flat feet or very high arches are also more prone to plantar fasciitis. The condition starts gradually with mild pain at the heel bone. You're more likely to feel it after (not during) exercise. The pain classically occurs again after arising from a midday lunch break. If you don't treat plantar fasciitis, it may become a chronic condition. You may not be able to keep up your level of activity and you may also develop symptoms of foot, knee, hip and back problems because of the way plantar fasciitis changes the way you walk.
Treatment for Plantar Fasciitis Rest is the first treatment for plantar fasciitis. Try to keep weight off your foot until the inflammation goes away. You can also apply ice to the sore area for 20 minutes three or four times a day to relieve your symptoms. Often a doctor will prescribe nonsteroidal anti-inflammatory medication such as ibuprofen. A program of home exercises to stretch your Achilles tendon and plantar fascia are the mainstay of treating the condition and lessening the chance of recurrence, along with proper arch supports. About 90 percent of people with plantar fasciitis improve significantly after two months of initial treatment. You may be advised to use shoes with shock-absorbing soles (like a walking or running shoe) or fitted with a temporary arch support. Your foot may also be taped into a specific position. If the taping or temporary arch supports are helpful, then you are a candidate for custom-molded arch supports, also called orthotics. If your plantar fasciitis is extremely swollen and tender, your doctor may inject your heel with steroidal anti-inflammatory medications (corticosteroid). If you still have symptoms, you may need to wear a walking cast for 2-3 weeks or positional splint when you sleep. In a few cases, you might need surgery to release your ligament.
Heel Spurs Patients with heel spurs usually have the same complaints as those with plantar fasciitis. This is due to the fact that the heel spur is actually a result of the continuous strain on the plantar fascia. Therefore, the treatment of heel spurs is the same as the treatment for plantar fasciitis. In about 10% of patients, the heel spur may be impinging on a nerve or may actually be fractured. Therefore, after exhausting the above-mentioned treatments, surgery may be necessary to remove the spur.
When your first few steps out of bed in the morning cause severe pain in the heel of your foot, you may have plantar fasciitis (fashee-EYE-tiss). It's an overuse injury affecting the sole or flexor surface (plantar) of the foot. A diagnosis of plantar fasciitis means you have inflamed the tough, fibrous band of tissue (fascia) connecting your heel bone to the base of your toes. You're more likely to get the condition if you're a woman, if you're overweight, or if you have a job that requires a lot of walking or standing on hard surfaces. You're also at risk if you walk or run for exercise, especially if you have tight calf muscles that limit how far you can flex your ankles. People with very flat feet or very high arches are also more prone to plantar fasciitis. The condition starts gradually with mild pain at the heel bone. You're more likely to feel it after (not during) exercise. The pain classically occurs again after arising from a midday lunch break. If you don't treat plantar fasciitis, it may become a chronic condition. You may not be able to keep up your level of activity and you may also develop symptoms of foot, knee, hip and back problems because of the way plantar fasciitis changes the way you walk.
Treatment for Plantar Fasciitis Rest is the first treatment for plantar fasciitis. Try to keep weight off your foot until the inflammation goes away. You can also apply ice to the sore area for 20 minutes three or four times a day to relieve your symptoms. Often a doctor will prescribe nonsteroidal anti-inflammatory medication such as ibuprofen. A program of home exercises to stretch your Achilles tendon and plantar fascia are the mainstay of treating the condition and lessening the chance of recurrence, along with proper arch supports. About 90 percent of people with plantar fasciitis improve significantly after two months of initial treatment. You may be advised to use shoes with shock-absorbing soles (like a walking or running shoe) or fitted with a temporary arch support. Your foot may also be taped into a specific position. If the taping or temporary arch supports are helpful, then you are a candidate for custom-molded arch supports, also called orthotics. If your plantar fasciitis is extremely swollen and tender, your doctor may inject your heel with steroidal anti-inflammatory medications (corticosteroid). If you still have symptoms, you may need to wear a walking cast for 2-3 weeks or positional splint when you sleep. In a few cases, you might need surgery to release your ligament.
Heel Spurs Patients with heel spurs usually have the same complaints as those with plantar fasciitis. This is due to the fact that the heel spur is actually a result of the continuous strain on the plantar fascia. Therefore, the treatment of heel spurs is the same as the treatment for plantar fasciitis. In about 10% of patients, the heel spur may be impinging on a nerve or may actually be fractured. Therefore, after exhausting the above-mentioned treatments, surgery may be necessary to remove the spur.

Pain in Back of Heel
If you have pain behind your heel, you may have inflamed the area where the Achilles tendon inserts into the heel bone (retrocalcaneal bursitis). People often get this by running too much or wearing shoes that rub or cut into the back of the heel. Pain behind the heel may build slowly over time, causing the skin to thicken, get red and swell.
Read More
You might also develop a bump on the back of your heel that feels tender and warm to the touch (Haglund's deformity). The pain flares up when you first start an activity after resting. It often hurts too much to wear normal shoes. You may need an X-ray to see if you also have a bone spur. Treatment includes resting from the activities that caused the problem, non-steroidal anti-inflammatory medication and wearing heel lifts or open back shoes. If your heel pain is not getting better with conservative treatment, then a surgical procedure may be necessary to remove the bump or bone spurs.
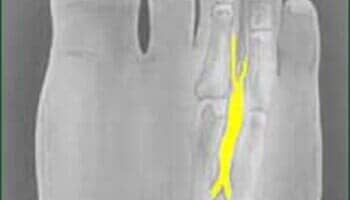
Neuromas
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. It occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
Read More
Signs and Symptoms Normally, there are no outward signs, such as a lump, because this is not really a tumor. The chief complaint is usually burning pain in the ball of the foot that radiates into the toes. The pain generally intensifies with activity or wearing shoes. Night pain is rare. There may also be numbness in the toes, or an unpleasant feeling in the toes. Runners may feel pain as they push off from the starting block. High-heeled shoes, which put the foot in a similar position to the push-off, can also aggravate the condition. Tight, narrow shoes also aggravate this condition by compressing the toe bones and pinching the nerve.
Diagnosis and Treatment During the examination, your physician will feel for a palpable mass or a "click" between the bones. They will put pressure on the spaces between the toe bones to try to replicate the pain and look for calluses or evidence of stress fractures in the bones that might be the cause of the pain. Range of motion tests will rule out arthritis or joint inflammations. X-rays may be required to rule out a stress fracture or arthritis of the joints that join the toes to the foot. Initial therapies are nonsurgical and relatively simple. They can involve one or more of the following treatments:
• Changes in footwear. Avoid high heels or tight shoes, and wear wider shoes with lower heels and a soft sole. This enables the bones to spread out and may reduce pressure on the nerve, giving it time to heal.
• Orthotics. Custom shoe inserts and pads also help relieve irritation by lifting and separating the bones, reducing the pressure on the nerve.
• Injection. One or more injections of a corticosteroid medication can reduce the swelling and inflammation of the nerve, bringing some relief.
If conservative treatment does not relieve your symptoms, a simple surgery may be performed by your doctor at Chicago Foot Health Centers. Surgery can resect a small portion of the nerve or release the tissue around the nerve.
Diagnosis and Treatment During the examination, your physician will feel for a palpable mass or a "click" between the bones. They will put pressure on the spaces between the toe bones to try to replicate the pain and look for calluses or evidence of stress fractures in the bones that might be the cause of the pain. Range of motion tests will rule out arthritis or joint inflammations. X-rays may be required to rule out a stress fracture or arthritis of the joints that join the toes to the foot. Initial therapies are nonsurgical and relatively simple. They can involve one or more of the following treatments:
• Changes in footwear. Avoid high heels or tight shoes, and wear wider shoes with lower heels and a soft sole. This enables the bones to spread out and may reduce pressure on the nerve, giving it time to heal.
• Orthotics. Custom shoe inserts and pads also help relieve irritation by lifting and separating the bones, reducing the pressure on the nerve.
• Injection. One or more injections of a corticosteroid medication can reduce the swelling and inflammation of the nerve, bringing some relief.
If conservative treatment does not relieve your symptoms, a simple surgery may be performed by your doctor at Chicago Foot Health Centers. Surgery can resect a small portion of the nerve or release the tissue around the nerve.

Ankle Injuries
Ankle sprains are common injuries that occur when ligaments are stretched or torn. The ankle sprain is the most common athletic injury. Nearly 85% of ankle sprains occur laterally, or on the outside of ankle joints. Sprains on the inside ligaments are less common. Many sprains occur when participating in sports, or by twisting the ankle when walking on an uneven surface. Some individuals, due to their bone structure or foot type, are more prone to ankle sprains.
Read More
The ankle joint is made up of three bones. The bones are called the tibia, fibula, and talus. These bones form a socket in which the ankle joint moves. The tibia, fibula and talus are connected to each other by ligaments. When an ankle is sprained, a ligament is stretched, partially torn or completely torn.
Ankle sprain symptoms vary depending on severity. Often, the ankle is tender, swollen and discolored. The ankle can be quite painful to touch. Walking is usually hampered and may become difficult depending on the severity of the sprain. A feeling of instability may occur, especially in severe ankle sprains when ligaments are torn. Ankle sprains are classified by "types" and range from mild to moderate to severe. Classifying ankle sprains helps the physician diagnose the specific structures involved in the injury. This also helps determine appropriate treatment plans for each type of ankle sprain. Type I ankle sprain, the least severe, occurs when ligament fibers have been stretched or slightly torn. Type II sprain occurs when some of these fibers or ligaments are completely torn. Type III, the most severe, occurs when the entire ligament is torn and there is significant instability of the ankle joint.
Fractures of the ankle bone or outside the foot bone may be present after any type of ankle sprain. Fractures require immediate diagnosis and attention for appropriate treatment. Therefore, x-rays are required to evaluate all sprains. Occasionally, more sophisticated testing is necessary to examine soft tissue injuries. For example, computerized tomography (CT) and magnetic resonance imaging (MRI) give detailed views of the bone and soft tissue structures around the ankle joint. Once the diagnosis is made, the podiatric surgeon recommends appropriate therapy.
Treatment for Ankle Sprains Initial treatment includes rest, ice, compression and elevation (RICE). The "RICE" method promotes healing, decreases pain, and reduces swelling around the ankle joint. In more severe cases, non-weight bearing activities are encouraged and crutches may be recommended. Compression may be achieved with an elastic bandage, splint, short leg cast or brace, depending on severity. Compression eliminates motion around the ankle joint. The ability to walk or participate in other weight-bearing activities during the healing process depends on the severity or type of ankle sprain. This is determined by your doctor once the diagnosis is made. Most ankle sprains heal in three to eight weeks. In more severe cases, ligaments may require more healing time to promote ankle stability. Repeated ankle sprains may cause chronic instability, interfering with walking or sports activities. In this case, the physician may recommend a surgical procedure to tighten or create new ligaments around the ankle joint to re-establish stability of the ankle joint. Conservative treatment of many foot and ankle problems often promotes pain relief. For example, ankle strengthening exercises following the injury help prevent recurrence of injury. Most of these exercises can be done at home after appropriate instruction. Ankle supports and braces or taping around the ankle joint is especially helpful for individuals participating in sports.
Treatment for Ankle Fractures If the fracture is stable (without damage to the ligament or the ankle joint), it can be treated with a leg cast or brace. Initially, a long leg cast may be applied, which can later be replaced by a short walking cast. It takes at least six weeks for a broken ankle to heal, and it may be several months before you can return to sports at your previous competitive level. Your physician will probably schedule additional X-rays while the bones heal, to make sure those changes or pressures on the ankle don't cause the bones to shift. If the ligaments are also torn, or if the fracture created a loose fragment of bone that could irritate the joint, surgery may be required to "fix" the bones together so they will heal properly. The surgeon may use a plate, screws, staples or tension bands to hold the bones in place. Usually, there are few complications, although there is a higher risk among diabetic patients afterwards, the surgeon will prescribe a program of rehabilitation and strengthening. Ranges of motion exercises are important, but keeping weight off the ankle is just as important.
Ankle sprain symptoms vary depending on severity. Often, the ankle is tender, swollen and discolored. The ankle can be quite painful to touch. Walking is usually hampered and may become difficult depending on the severity of the sprain. A feeling of instability may occur, especially in severe ankle sprains when ligaments are torn. Ankle sprains are classified by "types" and range from mild to moderate to severe. Classifying ankle sprains helps the physician diagnose the specific structures involved in the injury. This also helps determine appropriate treatment plans for each type of ankle sprain. Type I ankle sprain, the least severe, occurs when ligament fibers have been stretched or slightly torn. Type II sprain occurs when some of these fibers or ligaments are completely torn. Type III, the most severe, occurs when the entire ligament is torn and there is significant instability of the ankle joint.
Fractures of the ankle bone or outside the foot bone may be present after any type of ankle sprain. Fractures require immediate diagnosis and attention for appropriate treatment. Therefore, x-rays are required to evaluate all sprains. Occasionally, more sophisticated testing is necessary to examine soft tissue injuries. For example, computerized tomography (CT) and magnetic resonance imaging (MRI) give detailed views of the bone and soft tissue structures around the ankle joint. Once the diagnosis is made, the podiatric surgeon recommends appropriate therapy.
Treatment for Ankle Sprains Initial treatment includes rest, ice, compression and elevation (RICE). The "RICE" method promotes healing, decreases pain, and reduces swelling around the ankle joint. In more severe cases, non-weight bearing activities are encouraged and crutches may be recommended. Compression may be achieved with an elastic bandage, splint, short leg cast or brace, depending on severity. Compression eliminates motion around the ankle joint. The ability to walk or participate in other weight-bearing activities during the healing process depends on the severity or type of ankle sprain. This is determined by your doctor once the diagnosis is made. Most ankle sprains heal in three to eight weeks. In more severe cases, ligaments may require more healing time to promote ankle stability. Repeated ankle sprains may cause chronic instability, interfering with walking or sports activities. In this case, the physician may recommend a surgical procedure to tighten or create new ligaments around the ankle joint to re-establish stability of the ankle joint. Conservative treatment of many foot and ankle problems often promotes pain relief. For example, ankle strengthening exercises following the injury help prevent recurrence of injury. Most of these exercises can be done at home after appropriate instruction. Ankle supports and braces or taping around the ankle joint is especially helpful for individuals participating in sports.
Treatment for Ankle Fractures If the fracture is stable (without damage to the ligament or the ankle joint), it can be treated with a leg cast or brace. Initially, a long leg cast may be applied, which can later be replaced by a short walking cast. It takes at least six weeks for a broken ankle to heal, and it may be several months before you can return to sports at your previous competitive level. Your physician will probably schedule additional X-rays while the bones heal, to make sure those changes or pressures on the ankle don't cause the bones to shift. If the ligaments are also torn, or if the fracture created a loose fragment of bone that could irritate the joint, surgery may be required to "fix" the bones together so they will heal properly. The surgeon may use a plate, screws, staples or tension bands to hold the bones in place. Usually, there are few complications, although there is a higher risk among diabetic patients afterwards, the surgeon will prescribe a program of rehabilitation and strengthening. Ranges of motion exercises are important, but keeping weight off the ankle is just as important.

Diabetic Foot Care
Because diabetes is a systemic disease affecting many different parts of the body, ideal case management requires a team approach. The podiatric physician, as an integral part of the treatment team, has documented success in the prevention of amputations, one of the most serious conditions that they treat. The key to amputation prevention in diabetic patients is early recognition and regular foot screenings, at least annually, from a podiatric physician. At Chicago Foot Health Centers, diabetic foot care and limb salvage is one of our specialties.
Read More
Foot problems are a leading cause of hospitalization for the eight million persons in the United States who have been identified as having diabetes mellitus. Expenditures related to diabetic foot problems total hundreds of millions of dollars annually. It is estimated that 15% of all diabetics will develop a serious foot condition at some time in their lives. Common problems include infection, ulceration, or gangrene that may lead, in severe cases, to amputation of a toe, foot or leg. Most of these problems are preventable through proper care and regular visits to your podiatric physician. At Chicago Foot Health Centers, we can provide information on foot inspection and care, proper footwear, and early recognition and treatment of foot conditions.
Causes of Foot Problems Foot problems in persons with diabetes are usually the result of three primary factors: neuropathy, poor circulation, and decreased resistance to infection. Also, foot deformities and trauma play major roles in causing ulcerations and infections in the presence of neuropathy or poor circulation.
• Neuropathy (Nerve Damage) Your ability to detect sensations or vibration may be diminished. Neuropathy allows injuries to remain unnoticed and untreated for lengthy periods of time. It may cause burning or sharp pains in feet and interfere with your sleep. Ironically, painful neuropathy may occur in combination with a loss of sensation. Neuropathy can also affect the nerves that supply the muscles in your feet and legs. This ‘motor neuropathy' can cause muscle weakness or loss of tone in the thighs, legs, and feet, and the development of hammertoes, bunions, and other foot deformities.
•. Poor Circulation Persons with diabetes often have circulation disorders (peripheral vascular disease) that can cause cramping in the calf or buttocks when walking. The symptoms can progress to severe cramping or pain at rest, with associated color and temperature changes (the feet may turn bright red when hanging down and constantly feel cold). Also, the skin may become shiny, thinned and easily damaged. A reduction in hair growth and a thickening of the toenails might also be present. Poor circulation, resulting in reduced blood flow to the feet, restricts delivery of oxygen and nutrients that are required for normal maintenance and repair. Healing of foot injuries, infection or ulceration is affected. Peripheral vascular bypass operations may avert lower extremity amputation
• Infection Persons with diabetes are generally more prone to infections than non-diabetic people. Due to deficiencies in the ability of white blood cells to defend against invading bacteria, diabetics have more difficulty in dealing with and mounting an immune response to the infection. Infections often worsen and may go undetected, especially in the presence of diabetic neuropathy or vascular disease. Often, the only sign of a developing infection is unexplained high blood sugar, even without fever. The combination of fever and high blood sugar often warns of a severe infection requiring hospitalization. Lesser degrees of infection are often treated on an outpatient basis.
Ulcers of the Foot An ulceration or ulcer is usually a painless sore at the bottom of the foot or top of the toes, resulting from excessive pressure at that site. Ulcers frequently underlie a pre-existing corn or callus that was allowed to build up too thickly. Trauma from heat, cold, shoe pressure, or penetration by a sharp object is also potential causes. Neuropathy allows the lesions to develop because the normal warning sense of pain has been lost and they go unrecognized. Continued pressure or walking on the injured skin creates even further damage and the ulcer will worsen. The open sore will frequently become infected and may even penetrate to bone.
Treatment relies on early recognition of the ulceration by a podiatric physician, avoidance of weight-bearing activities such as walking, avoidance of wearing "closed-in" shoes, and early intervention. Besides local wound care, dressings and antibiotics, other measures may be necessary to adequately relieve pressure on the area. When use of crutches, a wheelchair, or rest is not feasible, plaster casts, braces, healing sandals, or orthoses (special shoe inserts) can be used to protect the foot while it heals. If circulation is inadequate to allow healing, your podiatric physician may refer you to a vascular surgeon for appropriate evaluation and possible vascular reconstructive surgery.
Once an ulcer has healed, it is important to continue to see your podiatric physician regularly. Special footwear and inserts may be recommended to protect your feet and prevent new or recurrent lesions from developing.
Foot Surgery in the Diabetic Patient Realizing the potential danger of foot deformities in the diabetic patient, corrective foot surgery is an option when you are in generally good health and have good circulation. Most deformities progressively worsen over time as do the effects of neuropathy and vascular or circulatory disease. When foot deformities cannot be managed effectively with conservative care, surgery may be indicated. Podiatric surgery is often "same day" surgery under local anesthesia to minimize potential complications. In some cases, such as in the presence of an active ulceration, hospitalization may be necessary to properly monitor your postoperative progress.
Surgery may also be required to heal an ulceration or to eradicate some infections, especially those involving the bone. Your cooperation is an important part of your care. You must guard against injury and provide the daily care necessary to maintain the health of your feet.
Footwear Guidelines Shoes must always fit comfortably and have adequate width and depth for the toes. Leather shoes easily adapt to the shape of your feet and allow them to "breathe." Athletic shoes, jogging shoes and sneakers are usually excellent choices if they are well fitted and provide adequate cushioning. Your podiatric surgeon may recommend "extra depth" shoes, custom molded shoes to adapt to your particular needs, or orthotics to provide cushioning and support.
• Always check your shoes for foreign objects or torn linings before putting them on.
•. New shoes should be worn for only a few hours at a time, and you should take care to inspect your feet for any points of irritation.
• Socks should be well fitted without seams or folds. They should not be so tight as to interfere with circulation. Well-padded socks can be very protective if there is an abundance of room in your shoes.
• Avoid wearing open-toed shoes or sandals until you have discussed this with your podiatric surgeon.
• Above all else, do not walk with bare feet. Foot Care Guidelines
• Inspect your feet daily for blisters, bleeding, and lesions between your toes.
•. Use a mirror to see the bottom of your foot and heel. If age or other factors hamper self-inspection, ask someone to help you.
• Do not soak your feet unless the temperature of the water is lukewarm, not as hot as you can stand it. (95°-100° Fahrenheit).
• Avoid temperature extremes - do not use hot water bottles or heating pads on your feet.
• Wash your feet daily with warm, soapy water and dry them well, especially between the toes.
• Use a moisturizing cream or lotion daily, but avoid getting it between the toes.
•. Do not use acids or chemical corn removers. Do not perform "bathroom surgery" on corns, calluses, or ingrown toenails.
• Trim your toenails carefully and file them gently.
• Have a podiatrist treat you regularly if you cannot trim them yourself without difficulty.
• Contact your podiatric physician immediately if your foot becomes swollen or is painful, or if redness occurs.
• Do not smoke. Tobacco can contribute to circulatory problems, which can be especially troublesome in patients with diabetes.
•. Learn all you can about diabetes and how it can affect your feet.
• A regular checkup by your podiatric physician—at least annually—is the best way to ensure that your feet remain healthy.
Causes of Foot Problems Foot problems in persons with diabetes are usually the result of three primary factors: neuropathy, poor circulation, and decreased resistance to infection. Also, foot deformities and trauma play major roles in causing ulcerations and infections in the presence of neuropathy or poor circulation.
• Neuropathy (Nerve Damage) Your ability to detect sensations or vibration may be diminished. Neuropathy allows injuries to remain unnoticed and untreated for lengthy periods of time. It may cause burning or sharp pains in feet and interfere with your sleep. Ironically, painful neuropathy may occur in combination with a loss of sensation. Neuropathy can also affect the nerves that supply the muscles in your feet and legs. This ‘motor neuropathy' can cause muscle weakness or loss of tone in the thighs, legs, and feet, and the development of hammertoes, bunions, and other foot deformities.
•. Poor Circulation Persons with diabetes often have circulation disorders (peripheral vascular disease) that can cause cramping in the calf or buttocks when walking. The symptoms can progress to severe cramping or pain at rest, with associated color and temperature changes (the feet may turn bright red when hanging down and constantly feel cold). Also, the skin may become shiny, thinned and easily damaged. A reduction in hair growth and a thickening of the toenails might also be present. Poor circulation, resulting in reduced blood flow to the feet, restricts delivery of oxygen and nutrients that are required for normal maintenance and repair. Healing of foot injuries, infection or ulceration is affected. Peripheral vascular bypass operations may avert lower extremity amputation
• Infection Persons with diabetes are generally more prone to infections than non-diabetic people. Due to deficiencies in the ability of white blood cells to defend against invading bacteria, diabetics have more difficulty in dealing with and mounting an immune response to the infection. Infections often worsen and may go undetected, especially in the presence of diabetic neuropathy or vascular disease. Often, the only sign of a developing infection is unexplained high blood sugar, even without fever. The combination of fever and high blood sugar often warns of a severe infection requiring hospitalization. Lesser degrees of infection are often treated on an outpatient basis.
Ulcers of the Foot An ulceration or ulcer is usually a painless sore at the bottom of the foot or top of the toes, resulting from excessive pressure at that site. Ulcers frequently underlie a pre-existing corn or callus that was allowed to build up too thickly. Trauma from heat, cold, shoe pressure, or penetration by a sharp object is also potential causes. Neuropathy allows the lesions to develop because the normal warning sense of pain has been lost and they go unrecognized. Continued pressure or walking on the injured skin creates even further damage and the ulcer will worsen. The open sore will frequently become infected and may even penetrate to bone.
Treatment relies on early recognition of the ulceration by a podiatric physician, avoidance of weight-bearing activities such as walking, avoidance of wearing "closed-in" shoes, and early intervention. Besides local wound care, dressings and antibiotics, other measures may be necessary to adequately relieve pressure on the area. When use of crutches, a wheelchair, or rest is not feasible, plaster casts, braces, healing sandals, or orthoses (special shoe inserts) can be used to protect the foot while it heals. If circulation is inadequate to allow healing, your podiatric physician may refer you to a vascular surgeon for appropriate evaluation and possible vascular reconstructive surgery.
Once an ulcer has healed, it is important to continue to see your podiatric physician regularly. Special footwear and inserts may be recommended to protect your feet and prevent new or recurrent lesions from developing.
Foot Surgery in the Diabetic Patient Realizing the potential danger of foot deformities in the diabetic patient, corrective foot surgery is an option when you are in generally good health and have good circulation. Most deformities progressively worsen over time as do the effects of neuropathy and vascular or circulatory disease. When foot deformities cannot be managed effectively with conservative care, surgery may be indicated. Podiatric surgery is often "same day" surgery under local anesthesia to minimize potential complications. In some cases, such as in the presence of an active ulceration, hospitalization may be necessary to properly monitor your postoperative progress.
Surgery may also be required to heal an ulceration or to eradicate some infections, especially those involving the bone. Your cooperation is an important part of your care. You must guard against injury and provide the daily care necessary to maintain the health of your feet.
Footwear Guidelines Shoes must always fit comfortably and have adequate width and depth for the toes. Leather shoes easily adapt to the shape of your feet and allow them to "breathe." Athletic shoes, jogging shoes and sneakers are usually excellent choices if they are well fitted and provide adequate cushioning. Your podiatric surgeon may recommend "extra depth" shoes, custom molded shoes to adapt to your particular needs, or orthotics to provide cushioning and support.
• Always check your shoes for foreign objects or torn linings before putting them on.
•. New shoes should be worn for only a few hours at a time, and you should take care to inspect your feet for any points of irritation.
• Socks should be well fitted without seams or folds. They should not be so tight as to interfere with circulation. Well-padded socks can be very protective if there is an abundance of room in your shoes.
• Avoid wearing open-toed shoes or sandals until you have discussed this with your podiatric surgeon.
• Above all else, do not walk with bare feet. Foot Care Guidelines
• Inspect your feet daily for blisters, bleeding, and lesions between your toes.
•. Use a mirror to see the bottom of your foot and heel. If age or other factors hamper self-inspection, ask someone to help you.
• Do not soak your feet unless the temperature of the water is lukewarm, not as hot as you can stand it. (95°-100° Fahrenheit).
• Avoid temperature extremes - do not use hot water bottles or heating pads on your feet.
• Wash your feet daily with warm, soapy water and dry them well, especially between the toes.
• Use a moisturizing cream or lotion daily, but avoid getting it between the toes.
•. Do not use acids or chemical corn removers. Do not perform "bathroom surgery" on corns, calluses, or ingrown toenails.
• Trim your toenails carefully and file them gently.
• Have a podiatrist treat you regularly if you cannot trim them yourself without difficulty.
• Contact your podiatric physician immediately if your foot becomes swollen or is painful, or if redness occurs.
• Do not smoke. Tobacco can contribute to circulatory problems, which can be especially troublesome in patients with diabetes.
•. Learn all you can about diabetes and how it can affect your feet.
• A regular checkup by your podiatric physician—at least annually—is the best way to ensure that your feet remain healthy.

Ingrown Toenails
Ingrown nails, the most common nail impairment, are nails whose corners or sides dig painfully into the soft tissue of nail grooves, often leading to irritation, redness, and swelling. Usually, toenails grow straight out. Sometimes, however, one or both corners or sides curve and grow into the flesh. The big toe is usually the victim of this condition, but other toes can also become affected.
Read More
An ingrown toenail may be caused by:
• Improperly trimmed nails (Trim then straight across, not longer than the tip of the toes. Do not round off corners. Use toenail clippers.)
• Heredity
• Shoe pressure; crowding of toes
• Repeated trauma to the feet from normal activities
If you suspect an infection due to an ingrown toenail, immerse the foot in a warm salt water soak, or a basin of soapy water, then apply an antiseptic and bandage the area. People with diabetes, peripheral vascular disease, or other circulatory disorders must avoid any form of self-treatment and seek podiatric medical care as soon as possible. Other "do-it-yourself" treatments, including any attempt to remove any part of an infected nail or the use of over-the-counter medications, should be avoided. Nail problems should be evaluated and treated by your podiatrist, who can diagnose the ailment, and then prescribe medication or another appropriate treatment.
At Chicago Foot Health Centers, we can resect the ingrown portion of the nail and may prescribe a topical or oral medication to treat the infection. If ingrown nails are a chronic problem, we can perform a procedure to permanently prevent ingrown nails. The corner of the nail that is ingrown, along with the matrix or root of that piece of nail, is removed by use of a chemical, a laser, or by other methods.
• Improperly trimmed nails (Trim then straight across, not longer than the tip of the toes. Do not round off corners. Use toenail clippers.)
• Heredity
• Shoe pressure; crowding of toes
• Repeated trauma to the feet from normal activities
If you suspect an infection due to an ingrown toenail, immerse the foot in a warm salt water soak, or a basin of soapy water, then apply an antiseptic and bandage the area. People with diabetes, peripheral vascular disease, or other circulatory disorders must avoid any form of self-treatment and seek podiatric medical care as soon as possible. Other "do-it-yourself" treatments, including any attempt to remove any part of an infected nail or the use of over-the-counter medications, should be avoided. Nail problems should be evaluated and treated by your podiatrist, who can diagnose the ailment, and then prescribe medication or another appropriate treatment.
At Chicago Foot Health Centers, we can resect the ingrown portion of the nail and may prescribe a topical or oral medication to treat the infection. If ingrown nails are a chronic problem, we can perform a procedure to permanently prevent ingrown nails. The corner of the nail that is ingrown, along with the matrix or root of that piece of nail, is removed by use of a chemical, a laser, or by other methods.

Nail Fungus
Fungal infection of the nail, or onychomycosis, is often ignored because the infection can be present for years without causing any pain. The disease is characterized by a progressive change in a toenail's quality and color, which is often ugly and embarrassing.
Read More
In reality, the condition is an infection underneath the surface of the nail caused by fungi. When the tiny organisms take hold, the nail often becomes darker in color and foul smelling. Debris may collect beneath the nail plate, white marks frequently appear on the nail plate, and the infection is capable of spreading to other toenails, the skin, or even the fingernails. If ignored, the infection can spread and possibly impair one's ability to work or even walk. This happens because the resulting thicker nails are difficult to trim and make walking painful when wearing shoes. Onychomycosis can also be accompanied by a secondary bacterial or yeast infection in or about the nail plate.
Because it is difficult to avoid contact with microscopic organisms like fungi, the toenails are especially vulnerable around damp areas where people are likely to be walking barefoot, such as swimming pools, locker rooms, and showers, for example. Injury to the nail bed may make it more susceptible to all types of infection, including fungal infection. Those who suffer from chronic diseases, such as diabetes, circulatory problems, or immune-deficiency conditions, are especially prone to fungal nails. Other contributing factors may be a history of athlete's foot and excessive perspiration.
Prevention
• Proper hygiene and regular inspection of the feet and toes are the first lines of defense against fungal nails • Clean and dry feet resist disease.
• Washing the feet with soap and water, remembering to dry thoroughly, is the best way to prevent an infection.
• Shower shoes should be worn when possible in public areas.
• Shoes, socks, or hosiery should be changed more than once daily.
• Toenails should be clipped straight across so that the nail does not extend beyond the tip of the toe.
• Wear shoes that fit well and are made of materials that breathe.
• Avoid wearing excessively tight hosiery, which promote moisture.
• Socks made of synthetic fiber tend to "wick" away moisture faster than cotton or wool socks.
• Disinfect instruments used to cut nails.
• Disinfect home pedicure tools.
• Don't apply polish to nails suspected of infection—those that are red, discolored, or swollen, for example.
Because it is difficult to avoid contact with microscopic organisms like fungi, the toenails are especially vulnerable around damp areas where people are likely to be walking barefoot, such as swimming pools, locker rooms, and showers, for example. Injury to the nail bed may make it more susceptible to all types of infection, including fungal infection. Those who suffer from chronic diseases, such as diabetes, circulatory problems, or immune-deficiency conditions, are especially prone to fungal nails. Other contributing factors may be a history of athlete's foot and excessive perspiration.
Prevention
• Proper hygiene and regular inspection of the feet and toes are the first lines of defense against fungal nails • Clean and dry feet resist disease.
• Washing the feet with soap and water, remembering to dry thoroughly, is the best way to prevent an infection.
• Shower shoes should be worn when possible in public areas.
• Shoes, socks, or hosiery should be changed more than once daily.
• Toenails should be clipped straight across so that the nail does not extend beyond the tip of the toe.
• Wear shoes that fit well and are made of materials that breathe.
• Avoid wearing excessively tight hosiery, which promote moisture.
• Socks made of synthetic fiber tend to "wick" away moisture faster than cotton or wool socks.
• Disinfect instruments used to cut nails.
• Disinfect home pedicure tools.
• Don't apply polish to nails suspected of infection—those that are red, discolored, or swollen, for example.

Athlete's Foot
Athlete's foot is a skin disease caused by a fungus, usually occurring between the toes. The fungus most commonly attacks the feet because shoes create a warm, dark, and humid environment which encourages fungus growth. The warmth and dampness of areas around swimming pools, showers, and locker rooms, are also breeding grounds for fungi. Because the infection was common among athletes who used these facilities frequently, the term "athlete's foot" became popular.
Read More
Not all fungus conditions are athlete's foot. Other conditions, such as disturbances of the sweat mechanism, reaction to dyes or adhesives in shoes, eczema, and psoriasis, also may mimic athlete's foot.
Symptoms
The signs of athlete's foot, singly or combined, are drying skin, itching scaling, inflammation, and blisters. Blisters often lead to cracking of the skin. When blisters break, small raw areas of tissue are exposed, causing pain and swelling. Itching and burning may increase as the infection spreads. Athlete's foot may spread to the soles of the feet and to the toenails. It can be spread to other parts of the body, notably the groin and underarms, by those who scratch the infection and then touch themselves elsewhere. The organisms causing athlete's foot may persist for long periods. Consequently, the infection may be spread by contaminated bed sheets or clothing to other parts of the body.
Prevention It is not easy to prevent athlete's foot because it is usually contracted in dressing rooms, showers, and swimming pool locker rooms where bare feet come in contact with the fungus. However, you can do much to prevent infection by practicing good foot hygiene. Daily washing of the feet with soap and water; drying carefully, especially between the toes; and changing shoes and hose regularly to decrease moisture, help prevent the fungus from infecting the feet. Also helpful is daily use of a quality foot powder.
Tips:
• Avoid walking barefoot; use shower shoes.
• Reduce perspiration by using talcum powder.
• Wear light and airy shoes.
• Wear socks that keep your feet dry, and change them frequently if you perspire heavily.
Treatment Fungicidal and fungistatic chemicals, used for athlete's foot treatment, frequently fail to contact the fungi in the horny layers of the skin. Topical or oral antifungal drugs are prescribed with growing frequency. In mild cases of the infection it is important to keep the feet dry by dusting foot powder in shoes and hose. The feet should be bathed frequently and all areas around the toes dried thoroughly. If an apparent fungus condition does not respond to proper foot hygiene and self-care, and there is no improvement within two weeks, seek professional treatment.
At Chicago Foot Health Centers, we will determine if a fungus is the cause of the problem. If it is, a specific treatment plan, including the prescription of antifungal medication, applied topically or taken by mouth, will usually be suggested. Such a treatment appears to provide better resolution of the problem, when the patient observes the course of treatment prescribed by the podiatrist; if it's shortened, failure of the treatment is common. If the infection is caused by a secondary bacterium, antibiotics, such as penicillin, that are effective against a broad spectrum of bacteria may be prescribed.
Treatment of Fungal Nails Treatments may vary, depending on the nature and severity of the infection. A daily routine of cleansing over a period of many months may temporarily suppress mild infections. White markings that appear on the surface of the nail can be filed off, followed by the application of an over-the-counter liquid antifungal agent. However, even the best over-the-counter treatments may not prevent a fungal infection from coming back.
At Chicago Foot Health Centers, we can detect a fungal infection early, culture the nail, determine the cause, and form a suitable treatment plan, which may include prescribing topical or oral medication, and debridement (removal of diseased nail matter and debris) of an infected nail. Newer oral antifungals, approved by the Food and Drug Administration, may be the most effective treatment. They offer a shorter treatment regimen of approximately three months and improved effectiveness. We may also prescribe a topical treatment for onychomycosis, which can be an effective treatment modality for fungal nails. In some cases, surgical treatment may be required. Temporary removal of the infected nail can be performed to permit direct application of a topical antifungal. Permanent removal of a chronically painful nail, which has not responded to any other treatment, permits the fungal infection to be cured and prevents the return of a deformed nail. Trying to solve the infection without the qualified help of a podiatric physician can lead to more problems. With new technical advances in combination with simple preventive measures, the treatment of this lightly regarded health problems can often be successful.
Symptoms
The signs of athlete's foot, singly or combined, are drying skin, itching scaling, inflammation, and blisters. Blisters often lead to cracking of the skin. When blisters break, small raw areas of tissue are exposed, causing pain and swelling. Itching and burning may increase as the infection spreads. Athlete's foot may spread to the soles of the feet and to the toenails. It can be spread to other parts of the body, notably the groin and underarms, by those who scratch the infection and then touch themselves elsewhere. The organisms causing athlete's foot may persist for long periods. Consequently, the infection may be spread by contaminated bed sheets or clothing to other parts of the body.
Prevention It is not easy to prevent athlete's foot because it is usually contracted in dressing rooms, showers, and swimming pool locker rooms where bare feet come in contact with the fungus. However, you can do much to prevent infection by practicing good foot hygiene. Daily washing of the feet with soap and water; drying carefully, especially between the toes; and changing shoes and hose regularly to decrease moisture, help prevent the fungus from infecting the feet. Also helpful is daily use of a quality foot powder.
Tips:
• Avoid walking barefoot; use shower shoes.
• Reduce perspiration by using talcum powder.
• Wear light and airy shoes.
• Wear socks that keep your feet dry, and change them frequently if you perspire heavily.
Treatment Fungicidal and fungistatic chemicals, used for athlete's foot treatment, frequently fail to contact the fungi in the horny layers of the skin. Topical or oral antifungal drugs are prescribed with growing frequency. In mild cases of the infection it is important to keep the feet dry by dusting foot powder in shoes and hose. The feet should be bathed frequently and all areas around the toes dried thoroughly. If an apparent fungus condition does not respond to proper foot hygiene and self-care, and there is no improvement within two weeks, seek professional treatment.
At Chicago Foot Health Centers, we will determine if a fungus is the cause of the problem. If it is, a specific treatment plan, including the prescription of antifungal medication, applied topically or taken by mouth, will usually be suggested. Such a treatment appears to provide better resolution of the problem, when the patient observes the course of treatment prescribed by the podiatrist; if it's shortened, failure of the treatment is common. If the infection is caused by a secondary bacterium, antibiotics, such as penicillin, that are effective against a broad spectrum of bacteria may be prescribed.
Treatment of Fungal Nails Treatments may vary, depending on the nature and severity of the infection. A daily routine of cleansing over a period of many months may temporarily suppress mild infections. White markings that appear on the surface of the nail can be filed off, followed by the application of an over-the-counter liquid antifungal agent. However, even the best over-the-counter treatments may not prevent a fungal infection from coming back.
At Chicago Foot Health Centers, we can detect a fungal infection early, culture the nail, determine the cause, and form a suitable treatment plan, which may include prescribing topical or oral medication, and debridement (removal of diseased nail matter and debris) of an infected nail. Newer oral antifungals, approved by the Food and Drug Administration, may be the most effective treatment. They offer a shorter treatment regimen of approximately three months and improved effectiveness. We may also prescribe a topical treatment for onychomycosis, which can be an effective treatment modality for fungal nails. In some cases, surgical treatment may be required. Temporary removal of the infected nail can be performed to permit direct application of a topical antifungal. Permanent removal of a chronically painful nail, which has not responded to any other treatment, permits the fungal infection to be cured and prevents the return of a deformed nail. Trying to solve the infection without the qualified help of a podiatric physician can lead to more problems. With new technical advances in combination with simple preventive measures, the treatment of this lightly regarded health problems can often be successful.

Plantar Warts
Warts are one of several soft tissue conditions of the foot that can be quite painful. They are caused by a virus, which generally invades the skin through small or invisible cuts and abrasions. They can appear anywhere on the skin, but, technically, only those on the sole are properly called plantar warts. Children, especially teenagers, tend to be more susceptible to warts than adults; some people seem to be immune.
Read More
Most warts are harmless, even though they may be painful. They are often mistaken for corns or calluses—which are layers of dead skin that build up to protect an area which is being continuously irritated. The wart, however, is a viral infection. Plantar warts tend to be hard and flat, with a rough surface and well-defined boundaries; warts are generally raised and fleshier when they appear on the top of the foot or on the toes. Plantar warts are often gray or brown (but the color may vary), with a center that appears as one or more pinpoints of black. It is important to note that warts can be very resistant to treatment and have a tendency to reoccur.
Source of the Virus The plantar wart is often contracted by walking barefoot on dirty surfaces or littered ground where the virus is lurking. The causative virus thrives in warm, moist environments, making infection a common occurrence in communal bathing facilities. If left untreated, warts can grow to an inch or more in circumference and can spread into clusters of several warts; these are often called mosaic warts. Like any other infectious lesion, plantar warts are spread by touching, scratching, or even by contact with skin shed from another wart. The wart may also bleed another route for spreading. Occasionally, warts can spontaneously disappear after a short time, and, just as frequently, they can recur in the same location. When plantar warts develop on the weight-bearing areas of the foot—the ball of the foot, or the heel, for example—they can be the source of sharp, burning pain. Pain occurs when weight is brought to bear directly on the wart, although pressure on the side of a wart can create equally intense pain.
Tips for Prevention:
• Avoid walking barefoot, except on sandy beaches.
• Change shoes and socks daily.
• Keep feet clean and dry.
• Check children's feet periodically.
• Avoid direct contact with warts—from other persons or from other parts of the body.
• Do not ignore growths on, or changes in, your skin.
Self-Treatment
Self-treatment is generally not advisable. Over-the-counter preparations contain acids or chemicals that destroy skin cells, and it takes an expert to destroy abnormal skin cells (warts) without also destroying surrounding healthy tissue.
Self-treatment with such medications especially should be avoided by people with diabetes and those with cardiovascular or circulatory disorders. Never use them in the presence of an active infection.
Professional Treatment
At Chicago Foot Health Centers, it is possible that we will prescribe and supervise your use of a wart-removal preparation. More likely, however, removal of warts by a simple surgical procedure, performed under local anesthetic, may be indicated. The procedure can be performed under local anesthesia either in your podiatrist's office surgical setting or an outpatient surgery facility.
Source of the Virus The plantar wart is often contracted by walking barefoot on dirty surfaces or littered ground where the virus is lurking. The causative virus thrives in warm, moist environments, making infection a common occurrence in communal bathing facilities. If left untreated, warts can grow to an inch or more in circumference and can spread into clusters of several warts; these are often called mosaic warts. Like any other infectious lesion, plantar warts are spread by touching, scratching, or even by contact with skin shed from another wart. The wart may also bleed another route for spreading. Occasionally, warts can spontaneously disappear after a short time, and, just as frequently, they can recur in the same location. When plantar warts develop on the weight-bearing areas of the foot—the ball of the foot, or the heel, for example—they can be the source of sharp, burning pain. Pain occurs when weight is brought to bear directly on the wart, although pressure on the side of a wart can create equally intense pain.
Tips for Prevention:
• Avoid walking barefoot, except on sandy beaches.
• Change shoes and socks daily.
• Keep feet clean and dry.
• Check children's feet periodically.
• Avoid direct contact with warts—from other persons or from other parts of the body.
• Do not ignore growths on, or changes in, your skin.
Self-Treatment
Self-treatment is generally not advisable. Over-the-counter preparations contain acids or chemicals that destroy skin cells, and it takes an expert to destroy abnormal skin cells (warts) without also destroying surrounding healthy tissue.
Self-treatment with such medications especially should be avoided by people with diabetes and those with cardiovascular or circulatory disorders. Never use them in the presence of an active infection.
Professional Treatment
At Chicago Foot Health Centers, it is possible that we will prescribe and supervise your use of a wart-removal preparation. More likely, however, removal of warts by a simple surgical procedure, performed under local anesthetic, may be indicated. The procedure can be performed under local anesthesia either in your podiatrist's office surgical setting or an outpatient surgery facility.

Children's Foot Issues
The doctors at Chicago Foot Health Centers are experts at addressing foot deformities in children, ranging from infants to teenagers. Below is some general information regarding children's feet.
Read More
A child's feet grow rapidly during their first year, reaching almost half their adult foot size. This is why foot specialists consider the first year to be the most important in the development of the feet. Here are some suggestions to help you assure that this development proceeds normally:
• Look carefully at your baby's feet. If you notice something that does not look normal to you, seek professional care immediately.
• Provide an opportunity for exercising the feet.
• Lying uncovered enables the baby to kick and perform other related motions which prepare the feet for weight-bearing.
• Change the baby's position several times a day. Lying too long in one spot, especially on the stomach, can put excessive strain on the feet and legs.
Starting to Walk It is unwise to force a child to walk. When physically and emotionally ready, the child will walk. Comparisons with other children are misleading, since the age for independent walking ranges from 10 to 18 months. When the child first begins to walk, shoes are not necessary indoors. Allowing the youngster to go barefoot or to wear just socks helps the foot to grow normally and to develop its musculature and strength, as well as the grasping action of toes. Of course, when walking outside or on rough surfaces, babies' feet should be protected in lightweight, flexible footwear made of natural materials.
Growing Up As a child's feet continue to develop, it may be necessary to change shoe and sock size every few months to allow room for the feet to grow. Although foot problems result mainly from injury, deformity, illness, or hereditary factors, improper footwear can aggravate preexisting conditions. Shoes or other footwear should never be handed down. The feet of young children are often unstable because of muscle problems which make walking difficult or uncomfortable.
Sports Activities Millions of American children participate in team and individual sports, many of them outside the school system, where advice on conditioning and equipment is not always available. Parents should be concerned about children's involvement in sports that require a substantial amount of running and turning, or involve contact. Protective taping of the ankles is often necessary to prevent sprains or fractures. Parents should consider discussing these matters with their family podiatrist if they have children participating in active sports. Sports-related foot and ankle injuries are on the rise as more children actively participate in sports.
Advice for Parents Problems noticed at birth will not disappear by themselves. You should not wait until the child begins walking to take care of a problem you've noticed earlier. Remember that lack of complaint by a youngster is not a reliable sign. The bones of growing feet are so flexible that they can be twisted and distorted without the child being aware of it. Walking patterns should be carefully observed. Does the child's toe point in or out, have knock knees, or other gait (walking) abnormalities? These problems can be corrected if they are detected early. Going barefoot is a healthy activity for children under the right conditions. However, walking barefoot on dirty pavements exposes children's feet to the dangers of infection through accidental cuts and to severe contusions, sprains or fractures. Another potential problem is plantar warts, a condition caused by a virus which invades the sole of the foot through cuts and breaks in the skin. They require protracted treatment and can keep children from school and other activities. Be careful about applying home remedies to children's feet, as many can cause irritation and damage to the feet.
• Look carefully at your baby's feet. If you notice something that does not look normal to you, seek professional care immediately.
• Provide an opportunity for exercising the feet.
• Lying uncovered enables the baby to kick and perform other related motions which prepare the feet for weight-bearing.
• Change the baby's position several times a day. Lying too long in one spot, especially on the stomach, can put excessive strain on the feet and legs.
Starting to Walk It is unwise to force a child to walk. When physically and emotionally ready, the child will walk. Comparisons with other children are misleading, since the age for independent walking ranges from 10 to 18 months. When the child first begins to walk, shoes are not necessary indoors. Allowing the youngster to go barefoot or to wear just socks helps the foot to grow normally and to develop its musculature and strength, as well as the grasping action of toes. Of course, when walking outside or on rough surfaces, babies' feet should be protected in lightweight, flexible footwear made of natural materials.
Growing Up As a child's feet continue to develop, it may be necessary to change shoe and sock size every few months to allow room for the feet to grow. Although foot problems result mainly from injury, deformity, illness, or hereditary factors, improper footwear can aggravate preexisting conditions. Shoes or other footwear should never be handed down. The feet of young children are often unstable because of muscle problems which make walking difficult or uncomfortable.
Sports Activities Millions of American children participate in team and individual sports, many of them outside the school system, where advice on conditioning and equipment is not always available. Parents should be concerned about children's involvement in sports that require a substantial amount of running and turning, or involve contact. Protective taping of the ankles is often necessary to prevent sprains or fractures. Parents should consider discussing these matters with their family podiatrist if they have children participating in active sports. Sports-related foot and ankle injuries are on the rise as more children actively participate in sports.
Advice for Parents Problems noticed at birth will not disappear by themselves. You should not wait until the child begins walking to take care of a problem you've noticed earlier. Remember that lack of complaint by a youngster is not a reliable sign. The bones of growing feet are so flexible that they can be twisted and distorted without the child being aware of it. Walking patterns should be carefully observed. Does the child's toe point in or out, have knock knees, or other gait (walking) abnormalities? These problems can be corrected if they are detected early. Going barefoot is a healthy activity for children under the right conditions. However, walking barefoot on dirty pavements exposes children's feet to the dangers of infection through accidental cuts and to severe contusions, sprains or fractures. Another potential problem is plantar warts, a condition caused by a virus which invades the sole of the foot through cuts and breaks in the skin. They require protracted treatment and can keep children from school and other activities. Be careful about applying home remedies to children's feet, as many can cause irritation and damage to the feet.

Geriatric Foot Issues
The human foot has been called the mirror of health. Foot doctors, or doctors of podiatric medicine (DPMs), are often the first doctors to see signs of such systemic conditions as diabetes, arthritis, and circulatory disease in the foot. Among these signs are dry skin, brittle nails, burning and tingling sensations, feelings of cold, numbness, and discoloration. Always seek professional care when these signs appear.
Read More
Foot Problems Can Be Prevented
For reasons that are difficult to fathom, many people, including a lot of older people, believe that it is normal for the feet to hurt, and simply resign themselves to enduring foot problems that could be treated. There are more than 300 different foot ailments. Some can be traced to heredity, but for an aging population, most of these ailments stem from the cumulative effect of years of neglect or abuse. However, even among people in their retirement years, many foot problems can be treated successfully, and the pain of foot ailments relieved. Whether due to neglect or abuse, the normal wear and tear of the years causes changes in feet. As persons age, their feet tend to spread, and lose the fatty pads that cushion the bottom of the feet. Additional weight can affect the bone and ligament structure. Older people, consequently, should have their feet measured for shoe sizes more frequently, rather than presuming that their shoe sizes remain constant. Dry skin and brittle nails are other conditions older people commonly face. Finally, it's a fact that women, young and old, have four times as many foot problems as men and high heels are often the culprits. Observing preventive foot health care has many benefits. Chief among them are that it can increase comfort, limit the possibility of additional medical problems, reduce the chances of hospitalization because of infection, and lessen requirements for other institutional care.
Foot Health Tips:
• Properly fitted shoes are essential; an astonishing number of people wear shoes that don't fit right, and cause serious foot problems.
• A shoe with a firm sole and soft upper is best for daily activities.
• Shop for shoes in the afternoon; feet tend to swell during the day.
• Walking is the best exercise for your feet.
• Pantyhose or stockings should be of the correct size and preferably free of seams.
• Do not wear constricting garters or tie your stockings in knots.
• Never cut corns and calluses with a razor, pocket knife, or other such instrument; use over-the-counter foot products only with the advice of a podiatrist.
• Bathe your feet daily in lukewarm (not hot) water, using a mild soap, preferably one containing moisturizers, or use a moisturizer separately.
• Test the water temperature with your hand.
• Trim or file your toenails straight across.
• Inspect your feet every day or have someone do this for you. If you notice any redness, swelling, cracks in the skin, or sores, consult your podiatrist.
For reasons that are difficult to fathom, many people, including a lot of older people, believe that it is normal for the feet to hurt, and simply resign themselves to enduring foot problems that could be treated. There are more than 300 different foot ailments. Some can be traced to heredity, but for an aging population, most of these ailments stem from the cumulative effect of years of neglect or abuse. However, even among people in their retirement years, many foot problems can be treated successfully, and the pain of foot ailments relieved. Whether due to neglect or abuse, the normal wear and tear of the years causes changes in feet. As persons age, their feet tend to spread, and lose the fatty pads that cushion the bottom of the feet. Additional weight can affect the bone and ligament structure. Older people, consequently, should have their feet measured for shoe sizes more frequently, rather than presuming that their shoe sizes remain constant. Dry skin and brittle nails are other conditions older people commonly face. Finally, it's a fact that women, young and old, have four times as many foot problems as men and high heels are often the culprits. Observing preventive foot health care has many benefits. Chief among them are that it can increase comfort, limit the possibility of additional medical problems, reduce the chances of hospitalization because of infection, and lessen requirements for other institutional care.
Foot Health Tips:
• Properly fitted shoes are essential; an astonishing number of people wear shoes that don't fit right, and cause serious foot problems.
• A shoe with a firm sole and soft upper is best for daily activities.
• Shop for shoes in the afternoon; feet tend to swell during the day.
• Walking is the best exercise for your feet.
• Pantyhose or stockings should be of the correct size and preferably free of seams.
• Do not wear constricting garters or tie your stockings in knots.
• Never cut corns and calluses with a razor, pocket knife, or other such instrument; use over-the-counter foot products only with the advice of a podiatrist.
• Bathe your feet daily in lukewarm (not hot) water, using a mild soap, preferably one containing moisturizers, or use a moisturizer separately.
• Test the water temperature with your hand.
• Trim or file your toenails straight across.
• Inspect your feet every day or have someone do this for you. If you notice any redness, swelling, cracks in the skin, or sores, consult your podiatrist.
Contact Information
Phone:
773-296-7160
Chicago Location:
3000 North Halsted Suite 801 Chicago, Illinois 60657
Tinley Park Location: 17019 Harlem Avenue, Tinley Park, Illinois 60477
Hours of Operation
- Sunday
- Closed
- Monday
- -
- Tuesday
- -
- Wed - Thu
- -
- Friday
- -
- Saturday
- -
Browse Our Website
Contact Information
Phone:
773-296-7160
Chicago Location:
3000 North Halsted Suite 801
Chicago, Illinois 60657
Tinley Park Location: 17019 Harlem Avenue, Tinley Park, Illinois 60477
Hours of Operation
- Sunday
- Closed
- Monday
- -
- Tuesday
- -
- Wed - Thu
- -
- Friday
- -
- Saturday
- -
Content, including images, displayed on this website is protected by copyright laws. Downloading, republication, retransmission or reproduction of content on this website is strictly prohibited. Terms of Use
| Privacy Policy
